New method paves the way for treatment of incurable brain cancer in children
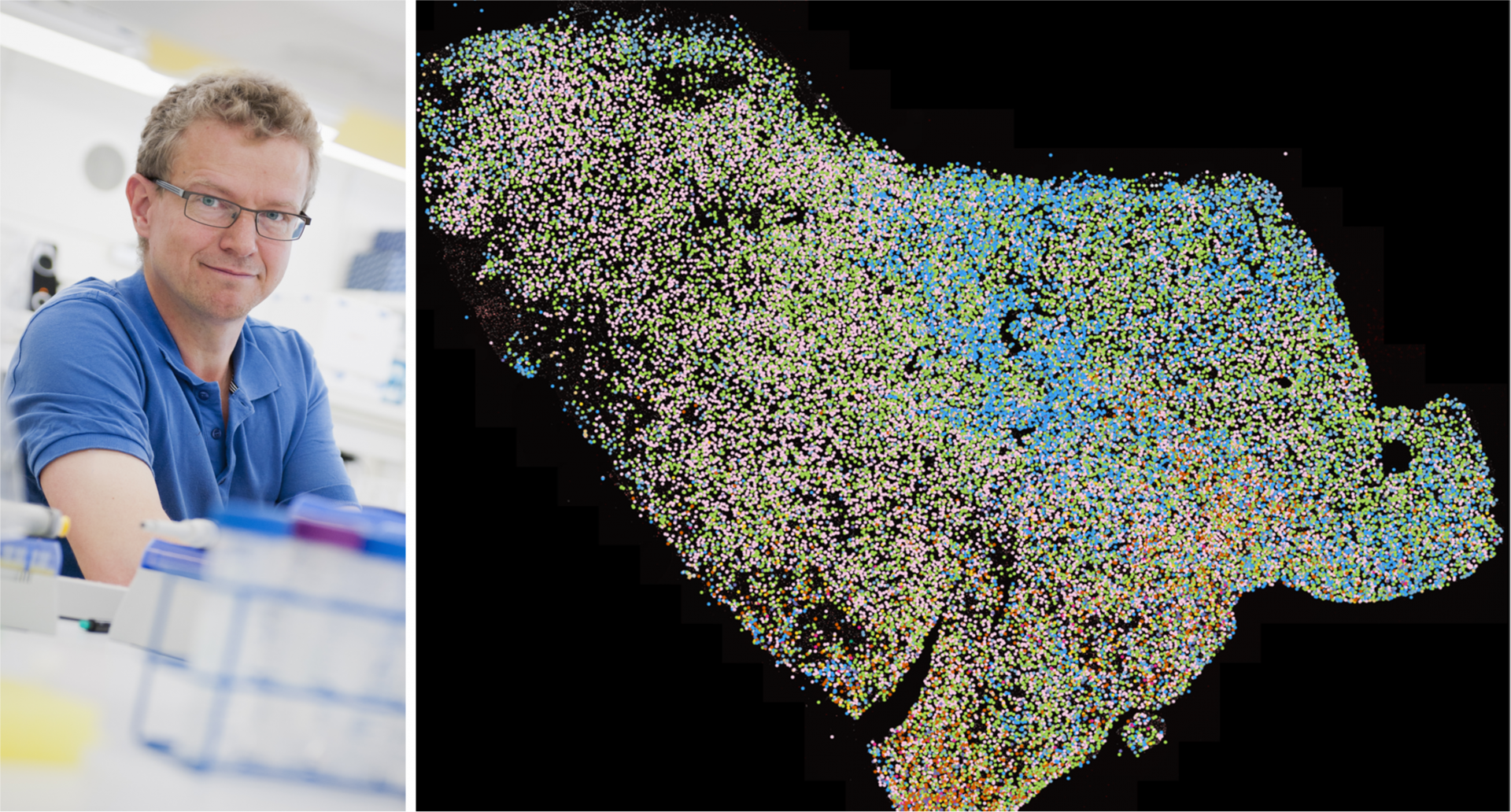
An international team of researchers, co-led by SciLifeLab researcher and Spatial and Single Cell Biology platform Director Mats Nilsson (Stockholm University), has found a way to visualize a rare cancer form called diffuse midline glioma, a type of cancer that is especially deadly for children who often die within a year after initial diagnosis. By visualizing the cancer cells, the team has now gained a better understanding of what the tumors look like. The hope is that it will lead to new treatment methods.
As of right now, there is no effective treatment for diffuse midline glioma, but by using spatial single-cell transcriptomics it is possible to see the structure of the tumor’s cancer cells, regardless of where it is situated or the age group of the patients. The study focused on age and location-dependent differences in diffuse midline gliomas by measuring genetic activity in 50 people between 2-68 years old.
“The problem with these types of tumors is that the cancer cells in them are very malleable. They have an ability to change shape into cells that resemble completely normal cells”, says Mats Nilsson, who co-led the study, in a press release from Stockholm University.
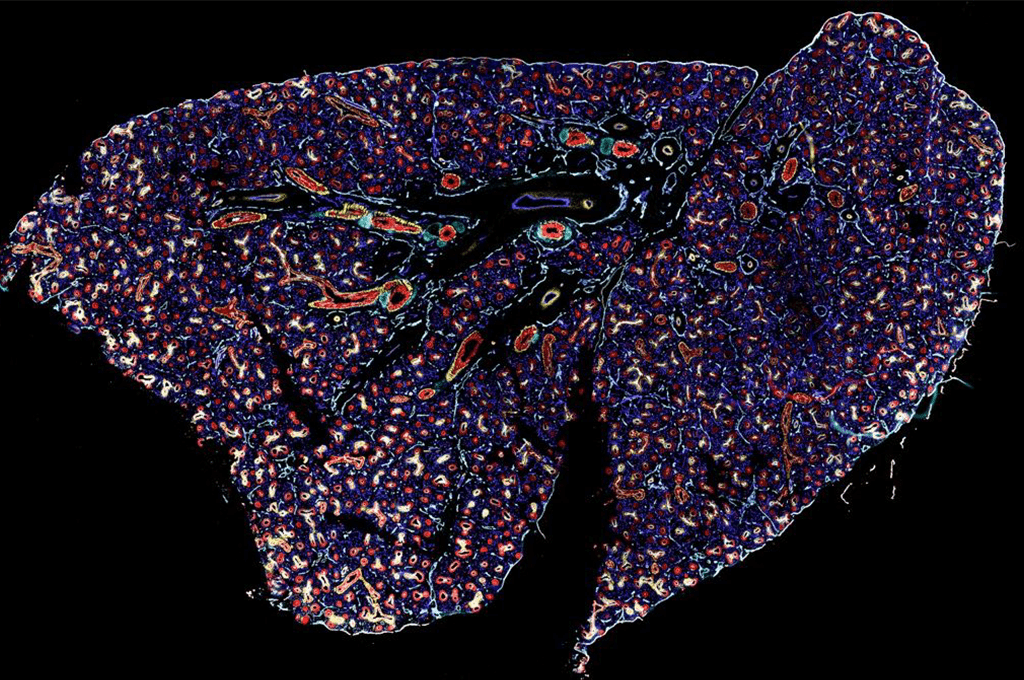
The research team were the first to discover that the spatial organization of cells could explain why the disease is so difficult to treat. The study, published in Nature Genetics, is the first to use spatially resolved single-cell technology on patient tissues, which emphasizes the need for specialized treatment based on the context of the tumor. The researchers focused on a particular genetic change called a Histone3-K27M mutation, which enables early stem cells of the brain to become cancerous.
By concentrating on the Histone3-K27M mutation the researchers found that pediatric tumors and tumors in the brainstem and spinal cord have more immature cells. These cells can multiply quickly and easily because of their similarity to stem cells. This might help explain why the disease is so deadly for younger children. Furthermore, they found that adult tumors have more mesenchymal-like cells that help heal damaged tissues but can also contribute to tumor growth and cancer progression. This difference could not be explained by any underlying genetic cause.
“By mapping the cells’ environments, we gain a better understanding of the circumstances under which the cells divide and thus also how we can try to disrupt this. Our part of the work at Stockholm University and SciLifeLab concerned the spatial part. We have created maps of tissue sections from a dozen tumors to see how the cells, identified in the study, are organized in the tumor tissue”, says Mats Nilsson.
The study suggests that children and adults diagnosed with diffuse midline gliomas might need different treatments.
When mapping out where the genetic activity was taking place to better understand the tumor’s structure and development, the researchers found something surprising. The cancer stem cells formed groups and surrounded themselves with a shield-like cell that protected the tumor.
Finding this structure helps come up with new ideas for treating diffuse midline glioma. By understanding how the cancer cells talk to each other and form this barrier, the treatment could be more targeted.
“With a better understanding of what it is that controls the cancer cells to resemble normal cells, you can try to develop treatment strategies that prevent them from being transformed in that way”, says Mats Nilsson.
Read the press release from Eurekalert